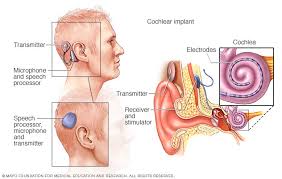
Indications and devices — Cochlear implants are surgically implanted prosthetic devices that electrically stimulate the cochlear nerve to provide hearing. The device consists of a battery-powered external processor (that looks like a hearing aid), a receiver coil implanted below the scalp, and an electrode inserted directly into the cochlea through a surgical opening.
The criteria for selecting cochlear implantation have expanded and continue to evolve. The minimum age for implantation has progressively dropped as implantation at an early age provides superior outcomes. In addition, bilateral implantation offers better sound localization and enhanced ability to understand speech in noisy environments. Deafened children with a variety of additional challenges such as inner ear malformation, cochlear nerve deficiency, and post meningitis cochlear ossification can also be successfully implanted, although candidacy must be individualized and post-implantation rehabilitation can be more challenging.
Cochlear implant devices (including those from Cochlea, Med-El, Advanced Bionics and Clarion) are approved by the US Food and Drug Administration for use in children as young as one year . A meta-analysis suggests that the role of cochlear implantation in children <12 months of age remains unclear since the literature is lacking in prospective studies or long-term follow-up. In children with postmeningitic deafness, earlier cochlear implantation may be warranted.
The advantage of early auditory stimulation during the “critical period” of hearing development needs to be balanced against the risks of the procedure.
Bilateral cochlear implants have been advocated as they allow a child to hear better in conditions with background noise (such as playgrounds and open classrooms), localize sound, and hear sound coming from either side without having to turn the head. Arguments against bilateral implantation include increased surgical and anesthetic risk, risk to residual hearing, and saving one ear for future technologies. If chosen, bilateral implants are either performed at one operative procedure or sequentially in separate surgeries. Studies demonstrate benefit from bilateral implantation with any length of time between surgeries. However, improved response at the brainstem and greater expressive language development is noted in patients with minimized duration between implants, with the greatest response seen in patients with simultaneous implantation.
Preoperative evaluation — Preoperative evaluation for a cochlear implant includes computed tomography or magnetic resonance imaging (MRI) of the temporal bone to evaluate the patency of the cochlea, identify congenital malformations, and assess surgical anatomy. Audiometric testing should be well documented. Other important prerequisites include access to an education program that stresses auditory and verbal skills and highly motivated parents who have realistic expectations. Because of the increased risk of meningitis in children with cochlear implants, immunization against Streptococcus pneumoniae, meningococcus and Haemophilus influenza is recommended.
Outcome — Cochlear implantation in children provides auditory detection over much of the speech signal and results in improved auditory discrimination and speech production. In one study, the language achievement of 29 prelingually deaf children three or more years after cochlear implantation was compared with the achievement of 29 prelingually deaf children who were treated with hearing aids. The children with cochlear implants had better language comprehension and production skills.
Children whose deafness occurs after age two years, who are deaf for short periods of time, who use oral communication, and/or who are implanted at an earlier age have the best language outcomes. As an example, the speech perception and production skills of three groups of children were analyzed after cochlear implantation: 70 children who were congenitally deaf, 22 children who were deafened by meningitis before two years of age, and 14 children who were deafened by meningitis after two years of age. The speech perception skills of the groups of children who were deafened after age two were better than those of the other two groups. No difference was found in speech perception or production skills between the two groups of children whose deafness began before age two years.
Speech perception was measured three, four, and five years after cochlear implantation in 40 children who were born deaf or who became deaf before three years of age and who had no measurable speech perception before implantation with the most powerful hearing aids. Speech perception improved with time (27, 35, and 45 mean words per minute at three, four, and five years of follow-up, respectively). Improvement in speech perception was greater for children who were younger at the time of implantation and who used oral, rather than total, communication (eg, including signing).
The language outcome may be poorer in children with underlying motor and/or , and in those with hypoplastic inner ear malformations and/or cochlear nerve deficiency. Severe inner ear dysplasia is also associated with a poorer audiologic outcome and increased surgical difficulty, including a higher rate of intraoperative cerebrospinal fluid gushers.
Educational and employment achievements were examined in a series of 100 prelingually deaf children who received cochlear implants before six years of age and were followed for at least four years after implantation .
Most children without additional disabilities were in mainstream schools. Approximately one-quarter experienced delayed reading and writing skills, and approximately one-half repeated a grade. Despite this, the educational and employment levels ultimately achieved in this group were comparable with that of their peers with normal hearing.
Cochlear implant failure, due to medical complications (infection or wound dehiscence) or device failure, is rare and is associated with a history of meningitis as the cause of deafness
Long-term follow-up — Patients with cochlear implants require lifelong follow-up to monitor for potential complications and to facilitate care if complications occur. In a meta-analysis of 88 studies including >22,000 adult and pediatric patients with cochlear implants, long-term complications occurred in 6 percent.
The most common complications included:
- Vestibular complications (eg, dizziness, balance problems) – 4 percent
- Device failure – 3 percent
- Taste problems – 3 percent
- Electrode problems – 2 percent
- Mastoiditis – 1.4 percent
- Skin infections – 1.3 percent
- Device rejection – 1.0 percent
- Seroma or hematoma – 0.9 percent
- Recurrent otitis – 0.8 percent
- Device migration – 0.7 percent
- Facial nerve palsy – 0.6 percent
- Cholesteatoma – 0.5 percent
The rates of postoperative and long-term complications do not appear to differ between children who undergo cochlear implantation at a young age (<12 months) compared with at a later age
Risk of meningitis — Children with cochlear implants are at increased risk for meningitis, particularly pneumococcal meningitis. This issue is discussed in detail separately. Modification of activities — Patients with cochlear implants are able to participate in most sports. Patients must remove the external speech processor for activities including water sports and must be cautious of their lack of hearing during these activities. Many advise against scuba diving because of rapid changes in pressure that may occur in the middle ear. Sports with the risk of head contact, such as kickboxing or wrestling, are also not advised, as they may disrupt the implant.
MRI may cause displacement of the internal magnet and can cause pain or discomfort in patients with cochlear implants. Some newer cochlear implants are MRI-safe, although the external processor must be removed. Other implants require a local surgical procedure to remove the internal magnet. The specific model of the cochlear implant and MRI machine must be verified to ensure the safety of the patient and implant prior to undergoing MRI.
